October 17, 2024
Nearly half of women over 40 have dense breast tissue, which is made of fibroglandular tissue and appears white on a mammogram. Breast density is determined from a mammogram, not a physical exam. There are 4 categories of breast density that are reported by the radiologist, and they are divided into quartiles based on the percentage of dense tissue showing on the mammogram.
In September of this year, the FDA began requiring mammography facilities to notify patients about the density of their breast tissue, labeling it “dense” or “not dense.” In addition, in the written report of mammography results sent to the healthcare provider, the facility is required to include an overall assessment of breast density, classified in 1 of the following categories:
- "The breasts are almost entirely fatty."
- "There are scattered areas of fibroglandular density."
- "The breasts are heterogeneously dense, which may obscure small masses."
- "The breasts are extremely dense, which lowers the sensitivity of mammography."

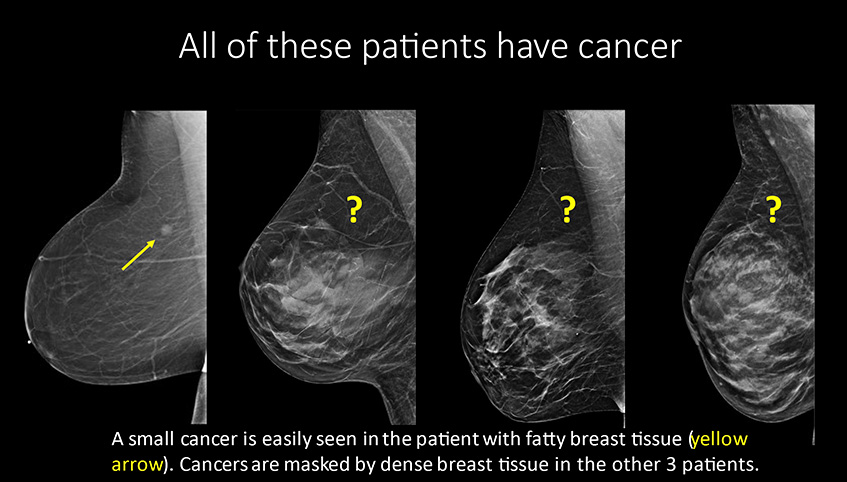
Dense breast tissue makes cancer more difficult to identify on a mammogram because white dense breast tissue can mask the cancer. Patients who have dense breast tissue are more likely to present with cancers that develop between screening intervals, larger tumors or later stage disease than patients who have less dense tissue.
Dense breast tissue is also an independent risk factor for breast cancer. Women with extremely dense breast tissue have a 4-fold greater risk of developing breast cancer than women with fatty breast tissue.
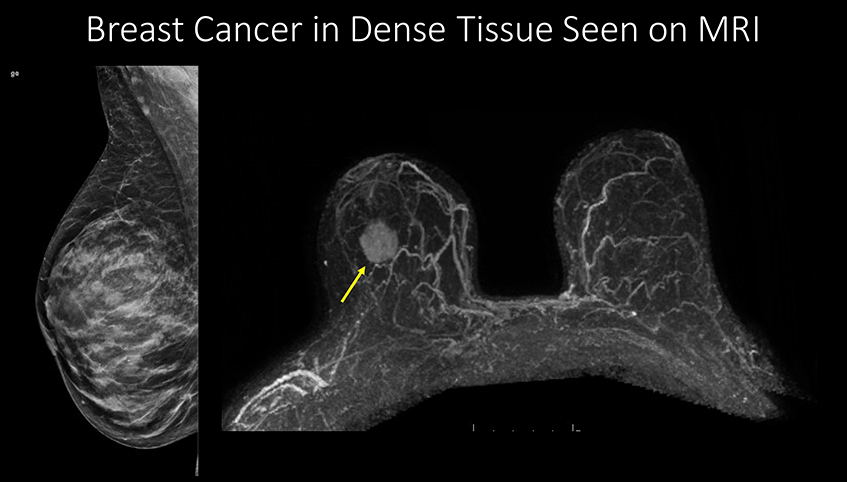
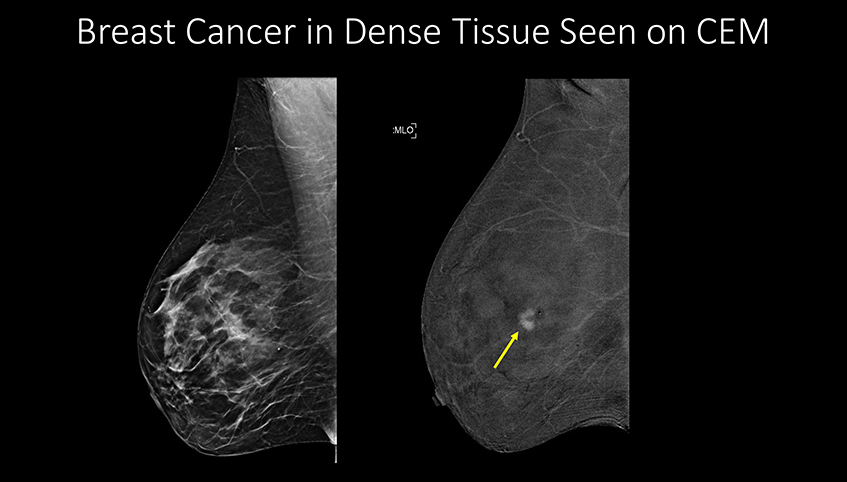
Breast MRI and CEM are more sensitive for breast cancer detection than ultrasound. Breast MRI and CEM require placement of an IV and administering contrast. Unlike screening mammograms, and dependent upon the patient’s insurance coverage, there is likely to be out-of-pocket expense for supplemental screening exams.
The images below show cancers that were not visible on a mammogram but are easily identifiable when other testing modalities are used. These images show results using MRI, CEM and automated breast ultrasound (ABUS).
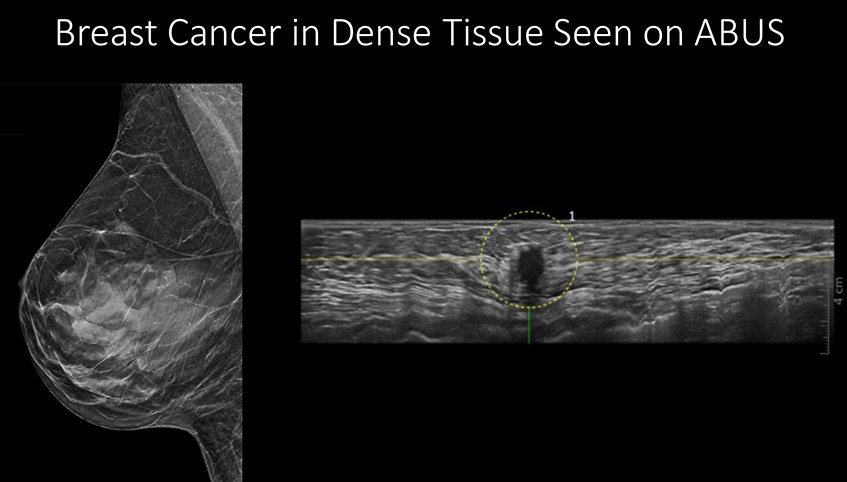
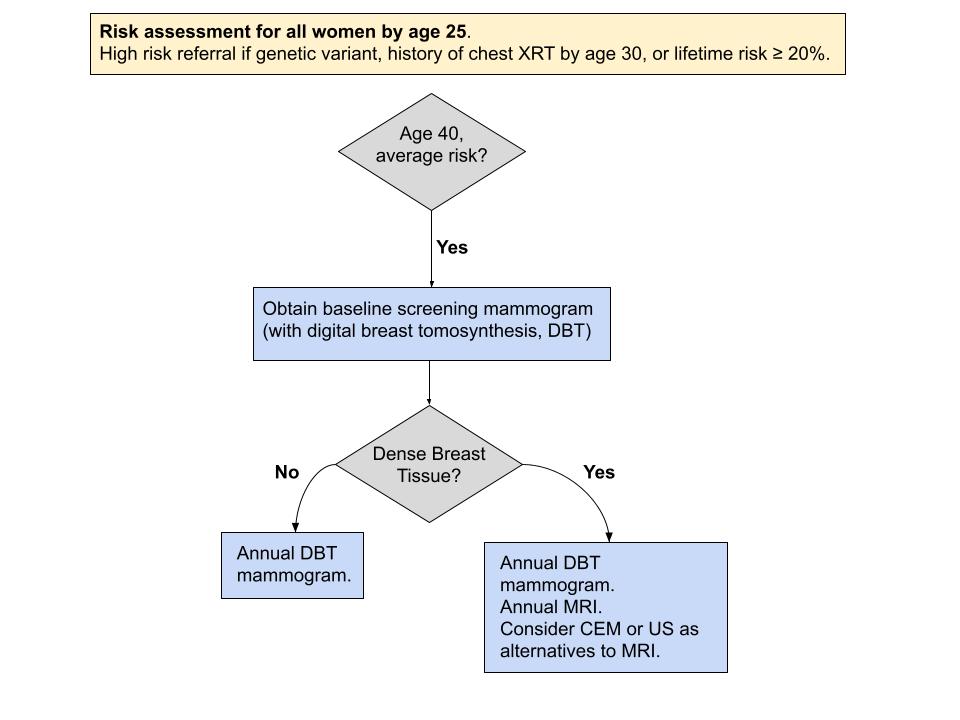
The University of Kansas Health System’s breast imaging program offers the largest variety of supplemental imaging services for patients with dense breast tissue. Imaging services available include abbreviated (limited) MRI, CEM, ABUS and hand-held ultrasound. The screening decision support tool below incorporates screening recommendations from the American College of Radiology. In addition, a printable chart provides additional details about breast cancer screening and diagnostic services offered at the health system.
Onalisa Winblad, MD, is certified by the American Board of Radiology. She completed a fellowship at the Mallinckrodt Institute of Radiology. She earned her medical degree from the University of Kansas School of Medicine and completed her residency at the University of Kansas Medical Center. She specializes in breast radiology.





